Overview
Cedar Heights Medical Center is a regional hospital that employs over 500 specialized healthcare professionals, including surgeons, nurses, anesthesiologists, and surgical technicians.
Each week, hospital administrators were tasked with building a complex schedule that matched the right people to the right procedures across 15 operating rooms.
This involved honoring strict licensing rules, managing time-off requests, balancing workloads, and responding to changing patient needs.
Legacy Manual Scheduling
Despite access to a modern HR system, the hospital still relied on a heavily manual scheduling process. It often led to staff burnout, last-minute conflicts, and underused operating room capacity.
Leaders at Cedar Heights knew that better planning could yield improvements across staff satisfaction, patient care, and operational efficiency.
Front Analytics helps organizations manages complex schedules across specialized staff and resource constrained facilities. Our AI-driven solutions are built to handle uncertainty, balance priorities, and optimize for real-world constraints. Contact us to learn how intelligent scheduling can elevate your operations.
The Challenge
Hospital administrators faced multiple competing priorities when building each week’s schedule. The system needed to:
- Satisfy all hard constraints, such as legal shift limits, credentialing requirements, and mandatory rest periods.
- Respect soft constraints like preferred shifts, weekend fairness, and continuity of care between patient and provider.
- Adapt quickly to last-minute changes such as unexpected absences or emergency surgical procedures.
- Reduce the burden on administrators who previously spent 40 or more hours each week coordinating assignments manually.
Existing tools were not equipped to handle these needs simultaneously. Leaders were forced to prioritize compliance at the expense of fairness, staff satisfaction, and flexibility.
Our Solution
Front Analytics built a multi-layered solution combining optimization, AI, and explainability.
Guaranteed to Solve all the Hard Rules
First, we developed a constraint solver using Google OR-Tools to guarantee that all hard rules were satisfied. This included licensing, maximum hours, room availability, and team composition rules.
Reinforcement Learning from Historic Data
Second, we introduced a reinforcement learning layer trained on three years of historical scheduling data. This layer helped maximize satisfaction of staff preferences without violating any core constraints.
Explainable
Third, we embedded a language model to explain and justify scheduling decisions. This made it easier for department heads to understand the logic behind each assignment and reduced the time required for manual review.
Re-optimize in Real Time
Finally, we added the ability to re-optimize the schedule in real time if something changed mid-week. This allowed the system to recover from disruptions without needing to rebuild the entire plan.
Business Value and Measurable Impact
Even though this exact example is not real, the results you could get would be. Imagine results like the following:
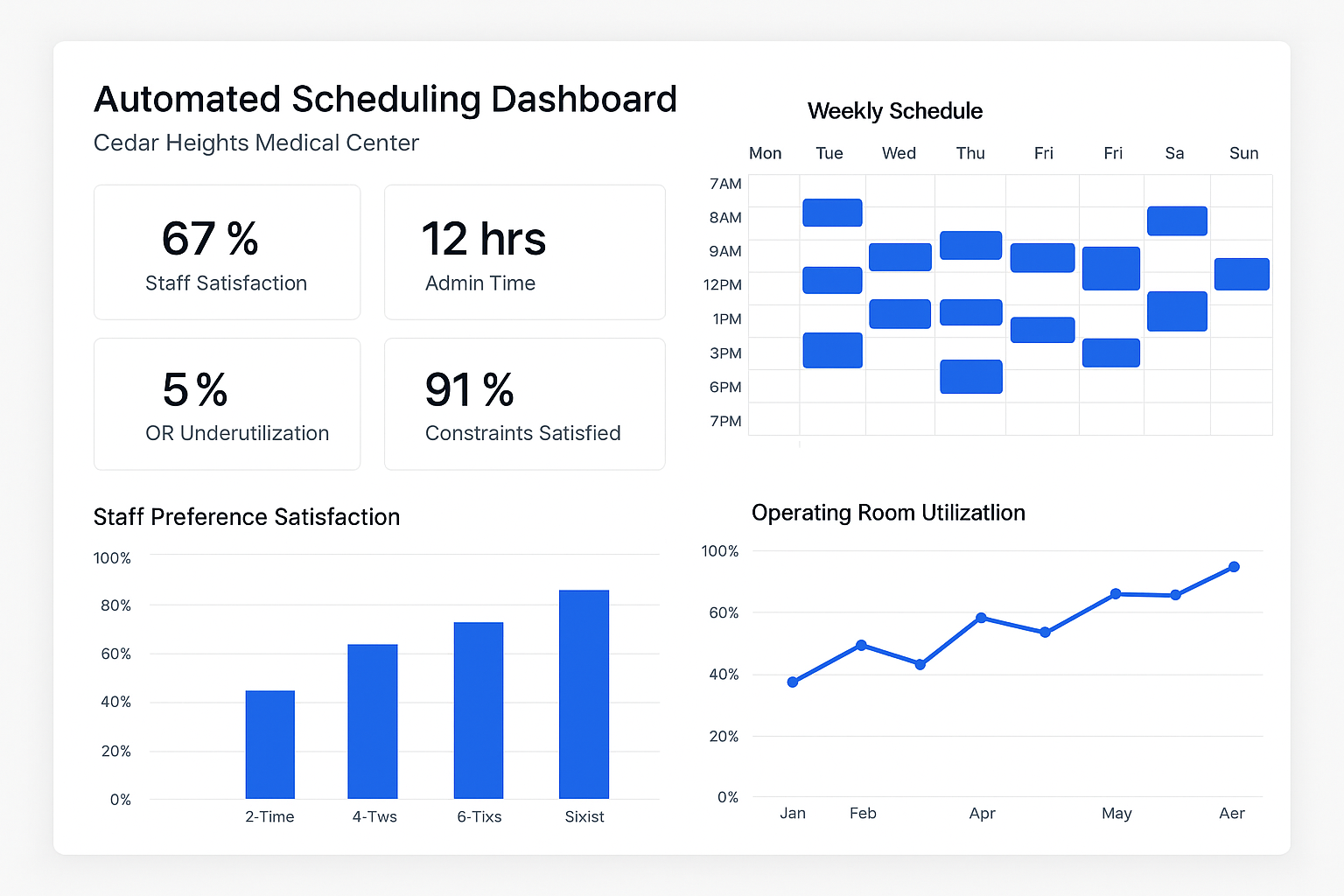
After just one quarter of use, Cedar Heights experienced major gains.
Staff satisfaction with the weekly schedule jumped from 67 percent to 91 percent. The number of manual adjustments required dropped from 80 to fewer than 15 per week.
Operating room idle time fell by more than half, and weekend shift distribution became significantly more balanced.
Perhaps most importantly, the scheduling burden on administrators decreased by over 85 percent, freeing them to focus on higher-value tasks.
One senior nurse commented that what used to take days of negotiation and frustration now gets done in a matter of hours, with far better outcomes for everyone involved.
Why It Matters
This case study illustrates the business value of using AI for operational decision-making.
At Cedar Heights, better scheduling translated into happier staff, higher patient throughput, and more efficient use of hospital resources.
Rather than replacing human judgment, the system amplified it.
Department leaders gained visibility, flexibility, and trust in the planning process. Patients benefited from greater continuity of care and fewer delays.
The organization as a whole became more resilient and responsive to change.