Hospitals run on dynamic systems: patient inflow surges, equipment fails unexpectedly, and staff availability shifts by the hour.
Weekly scheduling solves part of the puzzle, yet without continuous feedback the plan drifts as soon as reality changes.
A digital twin combined with model predictive control (MPC) offers a proactive answer.
The twin mirrors the live state of beds, staff, and operating rooms, while MPC recalculates corrective moves before small disruptions snowball into overtime and delayed care.
What Is a Digital Twin
A digital twin is a computational replica of a physical system that updates in near real time. In healthcare the twin tracks:
- Patient census and acuity on each ward
- Staff rosters, fatigue scores, and on‑call status
- Operating room slots, equipment availability, and maintenance windows
- Environmental signals such as inpatient admission trends or flu incidence
By constantly synchronizing with live data, the twin becomes a safe sandbox where planners can test scenarios before touching the real schedule.
Front Analytics specializes in designing and deploying these advanced planning systems. If you are ready to move beyond weekly rosters and embrace real‑time optimization, reach out to our team.
Adding Model Predictive Control
Model predictive control is a control‑theory method that looks ahead over a short horizon, optimizes an objective under constraints, then implements only the first action. At the next time step the process repeats with fresh data. When paired with a digital twin, MPC enables:
- Hourly or shift‑level rescheduling that respects hard rules
- Data driven trade‑offs between overtime cost, patient wait time, and staff fatigue
- Automatic adaptation to equipment outages or sudden surges in admissions
High‑Level Architecture
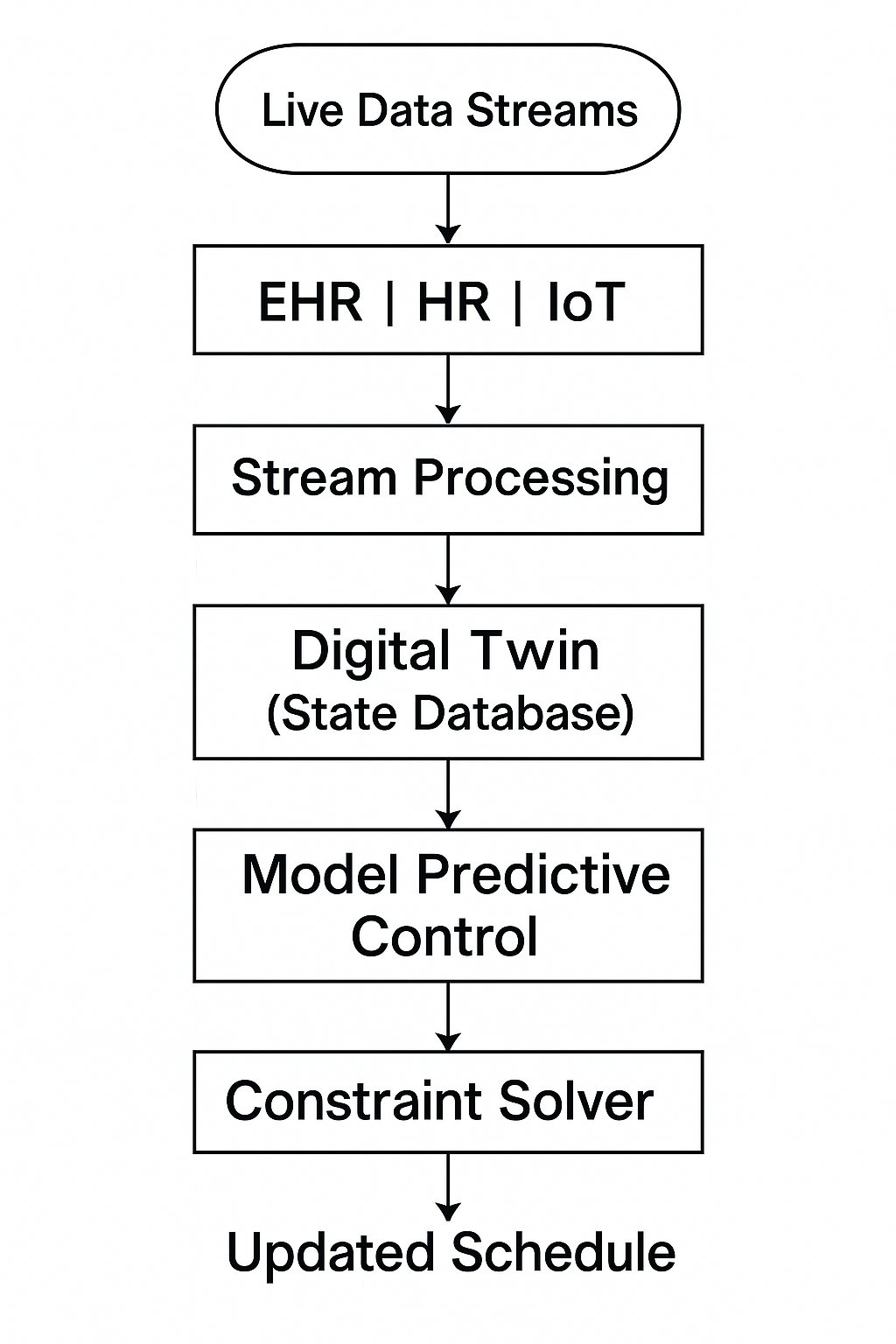
Key components
- Stream Processing: Normalizes and aggregates event data every few minutes.
- Digital Twin Storage: Time versioned database that stores current state and historical snapshots.
- MPC Engine: Python or Julia service running every hour with a rolling horizon of 6 to 12 hours.
- Constraint Solver: OR‑Tools or Gurobi instance that enforces licensing, rest periods, and room‑equipment matches.
4. Step‑by‑Step Implementation Guide
-
Data Integration
- Set up real‑time feeds from electronic health record, staff HR system, and operating room sensors.
- Use a schema registry so each source publishes consistent event types. -
Twin Modeling
- Define stock variables: available staff hours, open beds, idle OR minutes.
- Encode flow equations: admissions per hour, discharges, shift handoffs, equipment turnover.
- Validate the twin by replaying the last month and comparing to actual outcomes. -
Objective and Constraint Design
- Objectives: minimize overtime cost, minimize patient wait time, balance staff fatigue.
- Constraints: licensing rules, maximum consecutive hours, mandatory equipment sterilization gaps. -
Develop MPC Routine
- Horizon length: choose 6, 8, or 12 hours depending on volatility.
- At each cycle pull the latest twin state, forecast arrivals with a short term time series model, then call the solver.
- Apply only the first set of shift adjustments, store the rest as a candidate plan. -
Integration with Scheduler
- Publish adjustments as deltas: add this nurse to OR 3 for the next case, swap techs between OR 5 and OR 7.
- Notify supervisors via dashboard and allow a short manual review window. -
Monitoring and Feedback
- Track key performance indicators: response time to disruptions, avoided overtime hours, patient throughput.
- Feed realized outcomes back into the twin to correct drift.
5. Forecasting Inside the Twin
Short horizon forecasts give MPC a view of what is coming. Use:
- Exponential smoothing or Prophet for elective case volume when patterns are regular.
- Gradient boosting regressors with external features like day‑of‑week and season for admission surges.
- Kalman filter updates with sensor data from triage or ambulance intake for near real‑time noise reduction.
Accuracy is more important than complexity: forecasts need to be fast, interpretable, and sufficient for the next 6 to 12 hours.
6. Benefits to Expect
- Faster recovery from staff absences and equipment failures
- Reduction in overtime and agency spend
- Lower patient wait times for both bed placement and surgery starts
- Improved transparency because every reschedule action is linked to a forecast and a solver decision
7. Common Pitfalls
- Data latency: if streams lag, the twin becomes stale and MPC decisions misalign with reality.
- Overly long horizons: bigger horizons raise solve times and may incorporate outdated forecasts.
- Change management: staff must trust automated shift tweaks, so explainability dashboards are crucial.
8. Key Metrics for Ongoing Evaluation
- Mean time to reschedule after a disruption
- Hourly variance between twin state and real state
- Overtime hours per employee per week
- Operating room on time start percentage
- Number of manual overrides per day
Conclusion
A healthcare digital twin with model predictive control pushes scheduling from reactive to preventive.
By mirroring the system in real time and optimizing ahead of disruptions, hospitals gain resilience, lower cost, and better patient outcomes.
The approach is not limited to operating rooms. Any environment with specialized staff, strict rules, and volatile demand can benefit from the same architecture.